Published: 03/2023
Lean is a business methodology of process improvement focused on using a systematic approach to efficiency and effectiveness by eliminating waste. It has been increasingly incorporated into the healthcare industry over the last two decades. The core principle of Lean is identifying non-value-added activities and eliminating them creatively. “Lean thinking” can be an effective means to drive continuous quality improvement processes.
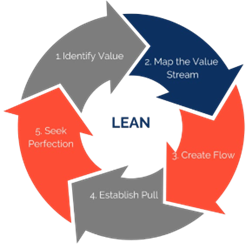
The term lean manufacturing was coined in the 1940’s-1950’s by Taiichi Ohno at Toyota and used as a post-war operational model to improve efficiency and eliminate waste in the automobile industry. Waste or “Muda” in Japanese is defined as unnecessary work that causes errors, disorganization, or poor communication. The 8 identified ‘Mudas” or areas of waste can be remembered using the acronym DOWNTIME: Defects, Overproduction, Waiting, Non-Utilized Talent, Transportation, Inventory, Motion, and Extra Processing. The term “Lean thinking” was later coined in the 1980’s by James Womack and Daniel Jones, who applied the general principles into an overall philosophy of management to create a continuous framework for improvement (Figure 1). The Lean Framework includes: (1) gathering stakeholders to identify value from the perspective of the customer, (2) mapping the current process, and (3) identifying the often-abundant waste within the existing process. Then, while focusing on the value stream to the customer, the stakeholders brainstorm and vet creative ways to improve flow, especially establishing “pull,” having the next step of the process available when the previous step is completed and pursue perfection by removing or revising steps that cause errors. Successful Lean improvements facilitate more effective and efficient team collaboration.
One example of the application of Lean and Lean Thinking Framework is the process of improving patient flow through in an ambulatory office (Table 1). The team focuses on the elimination of steps and processes that do not provide value to the patient. The goal of the LEAN process in this example is to reduce total time spent during clinic new patient appointments and increase patient provider caretime.
Figure 1: Lean Thinking Framework
| Lean Waste 8 Mudas | Examples of Waste in Outpatient Setting | Examples of Waste Correction |
|---|---|---|
| Defect | Not every new patient received a new patient packet Record releases not completed Multiple versions of the new patient intake form Arrival times vary for new patients | Creation of “New patient checklist” that includes sending of informational packet and release form Standardized new electronic medical record patient intake form Standardized scheduling of new patient appointments |
| Overproduction | Redundant request for patient demographic details including insurance type and Social Determinants of Health |
Standardized verification of patient information at check-in |
| Waiting | Unnecessary waiting times between clinical stations | Workflow changed to eliminate clinical stations by performing more tasks in the exam room (i.e., medication reconciliation, lab work, and check out process) |
| Non-utilized Talent | Missed opportunity for patients to complete history intake while in waiting area Missed opportunity for patients to read educational material in waiting room | Tablets/Forms given to patients at check-in to complete in waiting room Standardized educational material in waiting room |
| Transportation | Equipment storage far from actual rooms. Rooms are not designated for specific visits and therefore not properly stocked. |
Minimum supply list for stocking all rooms. Storage of specialized instruments in rooms for certain procedures (i.e., colposcopy, etc.) |
| Inventory | Lack of standardized checklist for supplies Delay in stocking supplies (orders only submitted when supply is exhausted) | Checklist of supplies and standard triggers established for inventory management |
| Motion | Inefficient storage of supplies and equipment (e.g., not having basic supplies/equipment in every examination room; staff searching for paperwork in various locations) |
Minimum supply list (including paperwork) for stocking all rooms Storage of specialized instruments in rooms for certain procedures (i.e., colposcopy, etc.) |
| Extra Processing | Unnecessary testing Unclear expectations leading to confusion and inefficiency in performing common tasks (e.g., specimen collection and labelling, giving injections, setting up procedures) | Creation of written protocols to standardize testing Clearly defined expectations, roles, and tasks based on assignments for nurses and nursing assistants |
Additional Readings
Going Lean in Health Care. IHI Innovation Series white paper. Cambridge, MA: Institute for Healthcare Improvement; 2005.
https://www.ihi.org/resources/Pages/IHIWhitePapers/GoingLeaninHealthCare.aspx.%20Retrieved%201 /24/23
https://www.ihi.org/resources/Pages/IHIWhitePapers/ComparingLeanandQualityImprovement.aspx.
Retrieved 1/24/23.